What is Prostate Cancer?
Prostate cancer is a form of cancer that occurs in the prostate, a small walnut-shaped gland in men that produces seminal fluid. It is one of the most common types of cancer in men. Early detection through prostate-specific antigen (PSA) tests and digital rectal exams can lead to successful treatment.
Why is Prostate Cancer Different for Gay and Bisexual Men?
What Are the Screening Disparities for Gay and Bisexual Men?
Studies indicate that gay and bisexual men are less likely to undergo regular prostate cancer screenings compared to their heterosexual counterparts. One study showed that gay men had lower odds of having an up-to-date PSA test (OR = 0.61) than heterosexual men. This disparity can be attributed to several factors:
- Stigma and Discrimination: Fear of discrimination in healthcare settings can deter GBT individuals from seeking regular medical care.
- Lack of Tailored Information: There is a shortage of prostate cancer educational resources specifically designed for gay and bisexual men.
Are Gay and Bisexual Men at Greater Risk for Prostate Cancer?
While gay and bisexual men are diagnosed with prostate cancer at similar rates to heterosexual men, certain lifestyle factors prevalent in the GBT community may influence their risk. These include:
- Use of Testosterone Supplements and Anabolic Steroids: Often used for muscle building, these can increase the risk of prostate cancer.
- HIV Status and Treatment: HIV-positive individuals, particularly those on antiretroviral therapy, may have different risk profiles for prostate cancer.
How Does Prostate Cancer Affect Transgender Women?
Prostate cancer is rare among transgender women, especially those who have undergone orchidectomy (removal of the testicles) or are on long-term hormone therapy. However, it is not entirely unheard of, and there are documented cases. The risk is largely influenced by the type and duration of hormone therapy and surgical procedures undergone.
What Are the Treatment Outcomes and Challenges for Gay and Bisexual Men?
How Does Prostate Cancer Treatment Impact Urinary and Bowel Function?
Gay and bisexual men often report poorer urinary and bowel outcomes after prostate cancer treatment compared to heterosexual men. The reasons for these differences are not entirely clear but may include:
- Differences in Sexual Practices: Receptive anal intercourse can complicate recovery and exacerbate issues related to urinary and bowel function.
- Communication Barriers: Gay and bisexual men might face challenges in discussing their sexual health with healthcare providers, leading to less optimal management of side effects.
How Does Prostate Cancer Treatment Affect Sexual Health in Gay and Bisexual Men?
Interestingly, gay and bisexual men report better sexual outcomes post-treatment compared to heterosexual men. This might be due to:
- Greater Openness and Innovation: Gay and bisexual men may be more willing to explore new ways to achieve sexual satisfaction post-treatment.
- Role Flexibility: Changes in sexual roles (e.g., switching from being the insertive partner to the receptive partner) may help maintain sexual intimacy.
What Are the Psychological Impacts of Prostate Cancer on GBT Individuals?
The psychological effects of prostate cancer and its treatment are profound for GBT individuals. They often experience:
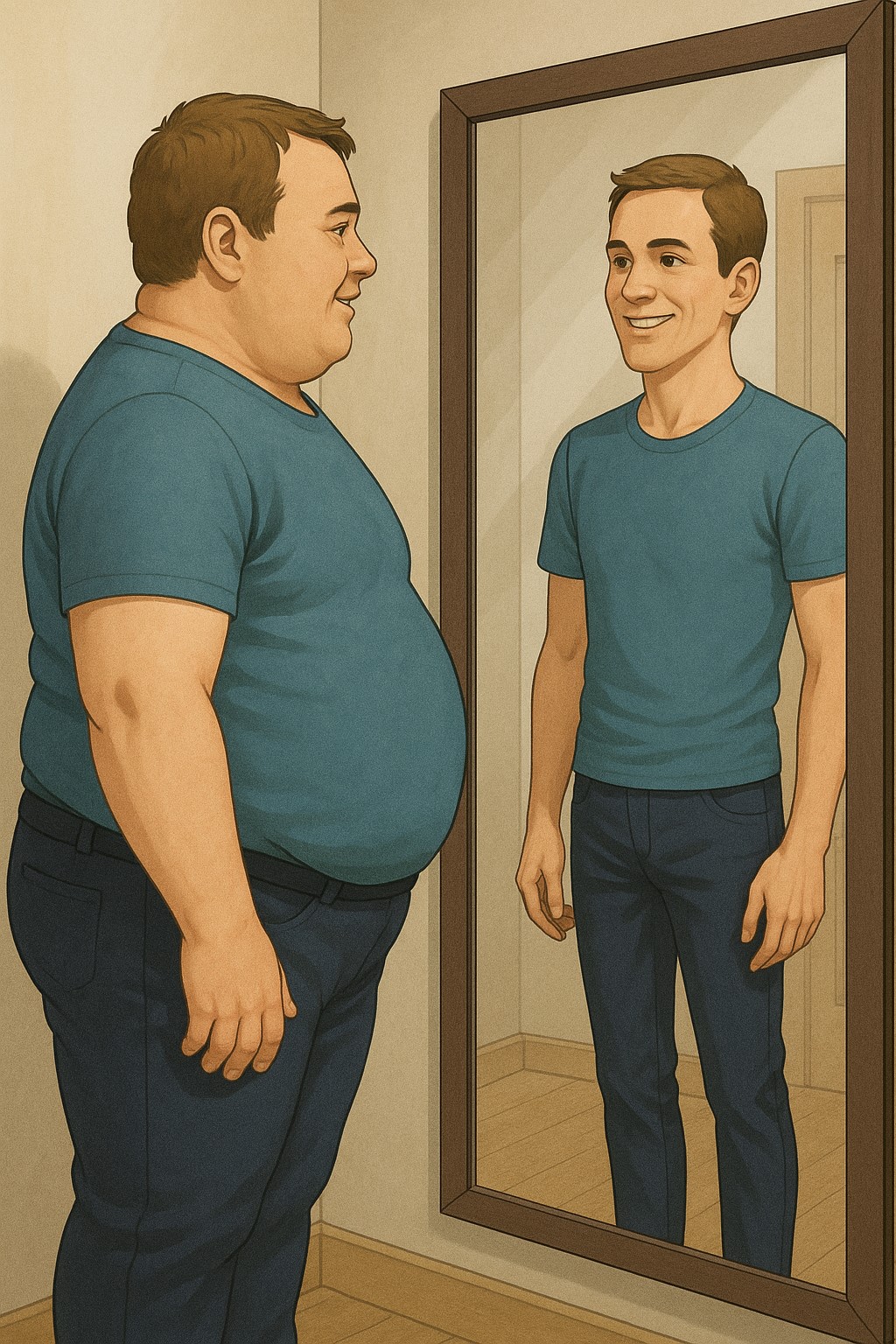
- Reduced Sense of Masculinity: The loss of sexual function can impact their gender identity and self-esteem.
- Stigma and Isolation: GBT individuals might face additional stigma related to both their sexual orientation and their cancer diagnosis, leading to feelings of isolation.
What Support Systems Are Available for GBT Individuals with Prostate Cancer?
GBT individuals typically have different support structures compared to heterosexual men. They are less likely to have a spouse or biological family for support and may rely more on friends or chosen family. Support groups specifically for GBT individuals with prostate cancer are beneficial but are often limited to larger cities.
What Can Be Done to Improve Care for GBT Individuals with Prostate Cancer?
To better support GBT individuals with prostate cancer, the following measures are recommended:
- Increase Awareness and Training: Healthcare providers should receive training on the unique needs of GBT patients.
- Develop Tailored Educational Resources: Creating prostate cancer information specifically for GBT individuals can help improve awareness and encourage regular screening.
- Enhance Communication: Encouraging open discussions about sexual health between GBT patients and their healthcare providers can lead to better management of treatment side effects.
Words of Wisdom from a Consultant Urologist
Prostate cancer affects men of all sexual orientations and gender identities, but understanding and addressing the unique needs of GBT individuals is crucial for improving outcomes. Regular screening, open communication with healthcare providers, and strong support systems are key to managing prostate cancer effectively. As we continue to research and understand these differences, we can provide more personalized and compassionate care to all patients.