What is the prostate gland?
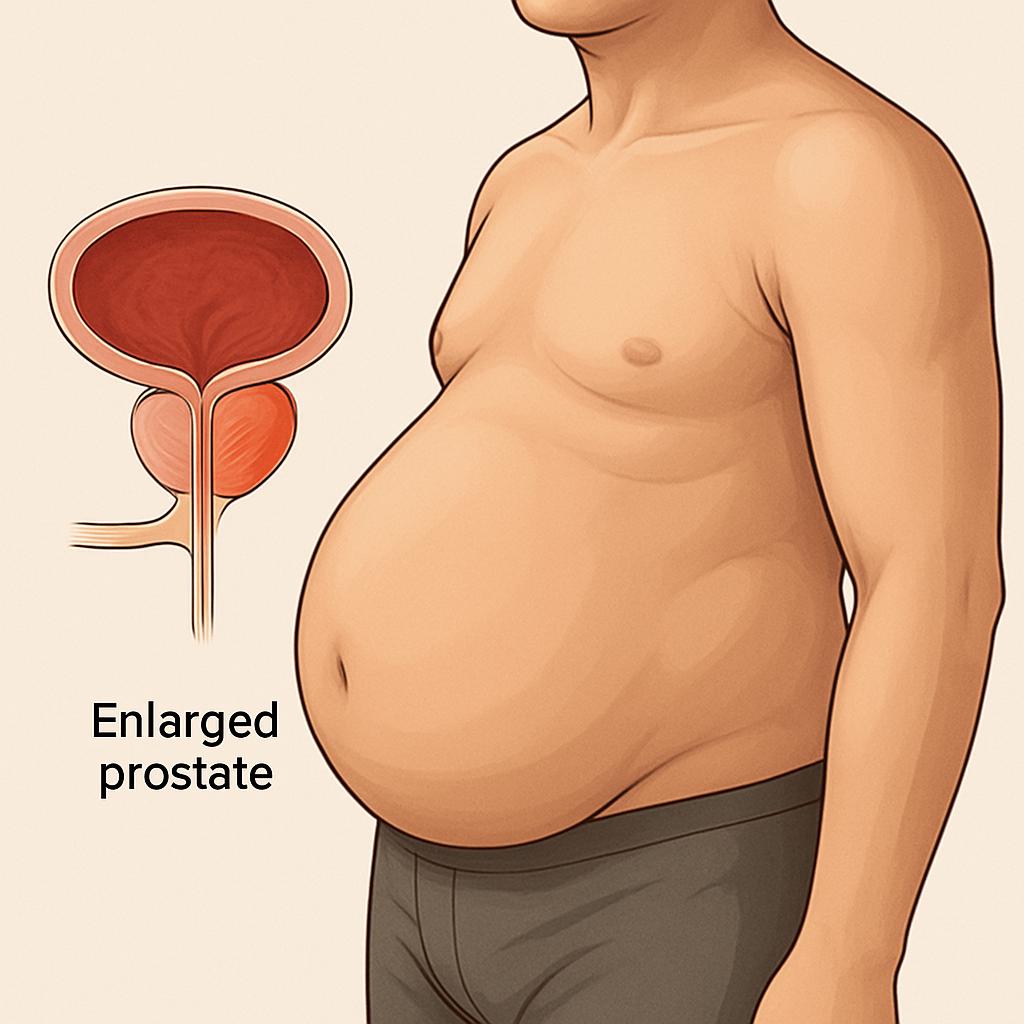
The prostate is a small, walnut-shaped gland that forms part of the male reproductive system. The production of prostate fluid is its primary function. This fluid is crucial to fertility as it nourishes and transports sperm.
The prostate gland is located below the bladder and enwraps the water pipe (the urethra carries urine from the bladder or, during orgasm, carries semen). The rectum forms part of the large bowel and lies behind the prostate gland.
What is benign prostatic hyperplasia?
When a doctor performs a digital rectal examination and finds an enlarged prostate, this is called benign prostate enlargement (BPE).
Benign prostatic hyperplasia is a diagnosis made only after prostate tissue is analysed, for example, after shaving of the prostate (TURP) or prostate biopsy. Often, the term is confused with benign prostatic hypertrophy, but this is an old error in the medical literature.
It's a common finding in men over 50 and tends to progress as they age.
In some men, the prostate grows only mildly; in others, it is more significant than expected, and in some, it can become huge. An enlarged prostate does not increase the risk of prostate cancer.
Why was I recommended a TURP?
You have been offered bladder outflow obstructive surgery (BOO) as your waterwork symptoms (lower urinary tract symptoms) have not responded to lifestyle and medical treatment.
What are the urine symptoms of an enlarged prostate?
- difficulty starting to pass urine
- a weak urine flow
- stop and start (stuttering) flow
- need to strain to pass urine or improve urine flow
- passing urine frequently
- nocturia: a need to wake up often at night to empty the bladder
- inability to hold urine
- the bladder is not emptied completely
What lifestyle changes are recommended?
- Switch to decaffeinated tea and decaffeinated coffee
- Lower the intake of fizzy drinks (including carbonated water), juices, spices
- Avoid artificial sweeteners
- The last drink before sleep time should be three hours before.
- Loose weight
- Ensure regular bowel habits
What medications are commonly prescribed?
- Alpha-blockers (tamsulosin, alfuzosin, and doxazosin) These medications relax the muscles in the bladder, neck, and urethra and help to improve urine flow.
- 5-Alpha reductase inhibitors (finasteride and dutasteride). These medications reduce, to some extent, the size of the gigantic prostate glands and, to a certain degree, in some cases, stop them from growing larger.
- Phosphodiesterase inhibitors (Cialis) These drugs are mainly prescribed for erectile issues. However, they were found to improve urinary problems by relaxing muscles in the lower urinary tract.
- Anticholinergics (solifenacin, oxybutynin, and trospium) relax the bladder muscles, reducing bladder spasms. They mainly address overactive bladder symptoms.
- Combination of the above medications. The above medicines are initially prescribed as a stand-alone; however, if BPH symptoms do not improve or bothersome symptoms worsen, a combination of drugs can be tried before considering surgical management.
What are the risks or complications of transurethral resection of the prostate?
- blood clot in the legs or lungs,
- chest or urine infection
- heart attack or stroke
- blood loss that may require a return back to the theatre or a blood transfusion
- Issues with bladder control (urinary frequency, urgency, or incontinence). If one is experiencing these troublesome symptoms, pelvic floor exercises, medications, or further surgery may be recommended.
- Some men (10%), even though the passage is wide, still experience urinary retention due to bladder wall weakness
- dry orgasms (the semen passes into the bladder instead of out through the water pipe), retrograde ejaculation.
- erectile problems (erectile dysfunction),
- waterpipe narrowing
- regrowth of the prostate
- TURP syndrome; is very rare nowadays.
Are there alternatives to TURP?
Transurethral resection of the prostate (TURP) is only one type of procedure for an enlarged prostate gland. Other options include the following.
- Holmium laser enucleation of the prostate (HoLEP). This uses a high-powered laser to remove part of your prostate.
- Transurethral vaporisation of the prostate (TUVP). This involves using an electrical current to burn away parts of your prostate.
- Photoselective vaporisation (PVP). This technique uses a particular laser, destroying prostate tissue without leaving any fragments behind. It's sometimes called 'Greenlight' laser surgery.
- Transurethral incision of the prostate (TUIP). This involves your surgeon making minor cuts in the neck of your bladder and prostate to widen the bladder opening., It may be an option if your prostate is only slightly enlarged.
- Open prostatectomy. This surgery removes part of your prostate through a cut in your abdomen (tummy) instead of going through the urethra. As a more invasive surgery, it's usually only suggested for a large prostate.
- UroLift. This is a less invasive option that may be offered for a smaller prostate. It involves a surgeon inserting a small implant to pull the tissue of the prostate away from the urethra, opening it up. One device approved for this procedure is called UroLift.
- Prostate artery embolisation. This procedure blocks the blood supply to your prostate gland, causing some of the tissue to die and shrinking your prostate. It's a less invasive option that might be suitable for some men.
- Rezum steam treatment. This involves using stream treatment to destroy part of your prostate. The steam is delivered to your prostate using an instrument inserted through your urethra.
Your surgeon will talk to you about the most suitable treatment. This will depend on several factors, including how severe your symptoms are, how big your prostate is, whether you have any other health problems and what's available at your local hospital.
How to preparing for TURP
- Lose weight
- If you smoke, stop smoking
- If you drink, lower your alcohol intake
- Eat healthily
- Increase your physical activity.
What you can expect on arrival
The ward nurse will complete all the documentation of your admission, ensure all the necessary information is correct, take a set of observations and provide you with a hospital gown and anti-thrombotic stocking.
Your anaesthetist will discuss general anaesthesia (you are put to sleep) and spinal anaesthetic (an injection is given in the back, and you will not feel anything from the waist down) options.
Your NHS consultant urological surgeon or private urologist will discuss the resection of the prostate surgery, hospital stay and complications. A written consent form is compiled.
You will be taken to the theatre.
What is transurethral resection of the prostate (TURP)?
TURP is a surgical procedure that cores the prostate gland, leaving the outer layer (prostate gland capsule) intact. This is performed under general anaesthesia or spinal anaesthesia.
This is done by introducing an extraordinary camera scope through which a loop can be passed.
An electrical current passes through the loop, and heat is generated. This is used to shave the enlarged prostate, widening the water pipe (urethra) channel and allowing better urine flow.
Resection of the prostate takes between 45 and 60 minutes, depending on your prostate size and surgeon experience.
Once the excess prostate tissue has been removed, any bleeding points in the prostate cavity are addressed.
The surgeon passes a thin tube called a catheter at the end of the prostate scraping surgery to drain urine.
Irrigating fluid is attached to the catheter to prevent blood clot formation that potentially blocks urine flow with serious complications which need further treatment.
Are incisions done during a TURP?
No. TURP is one of the many minimally invasive procedures. There are no skin cuts.
Is TURP a high-risk surgery?
No. TURP is not considered a high-risk surgery.
TURP is a commonly done procedure which is safe as the risk of severe complications is small.
What happens after surgery
Knowing what to expect after your surgery empowers you and lowers your anxiety.
The ward nurse checks you well and takes standard observations like blood pressure, pulse, breathing, temperature and oxygen level.
Is it normal to feel drowsy?
To feel giddy is normal after your anaesthesia. Many do not remember much about the first couple of hours.
Drips and tubes
After your surgery, you may have 1 or 2 tubes (vein cannulas). These give you fluids to keep you well hydrated or medications like painkillers, anti-sickness, etc.
A urinary catheter is introduced after a TURP. This thin tube passes through your water pipe into your bladder, so urine and blood or blood clots are drained into a collection bag.
The catheter was traditionally removed within 48 hours; however, nowadays, many urologists remove the catheter in 24 hours if your urine is clear.
Some men find difficulties passing urine when the catheter is removed. This is caused by swelling in the area where the shavings have been done, which impedes the passage of urine. A catheter needs to be placed back, and you will go home with a catheter. This remains for a couple of weeks until the swelling goes down. Then, you will be asked to come back to have the catheter removed.
Urinary symptoms after a TURP.
At first, one can experience a sudden urge (cannot hold urine), frequent urination and may leak some urine after a TURP. Week after week, this usually improves.
Will I be given a discharge letter?
Before you leave the hospital ward, you will be given a summary of your admission, medications you need to take, future follow-up dates, and essential contact details should you need assistance.
Will I receive an Enhanced Recovery approach?
The gold standard of care that every patient should receive after surgery is to be provided with an enhanced recovery programme.
You will be asked to;
- get out of bed and start walking as soon as possible to breathe better and lower the risk of clots in the deep veins or lungs,
- eat and drink after having an operation to encourage your bowel habits to kick start,
- perform breathing exercises to lower the risk of chest infection
- removing tubes or drains that are not needed to reduce the risk of infections
- wear your own clothes; this has a positive psychological effect
Recovering at home from TURP
TURP recovery takes around 6 weeks.
Drink plenty of fluids to flush out debris, bacteria and blood clots.
Avoid lifting heavy objects or involve yourself in heavy straining or strenuous exercise for a few weeks after the TURP to help prevent bleeding.
You may experience blood in your urine in the first few days. This should be light rose and quickly apparent in drinking water. Two weeks after the surgery, it is not uncommon to have blood in your urine. This is due to the lifting of the scab. If you increase your drinking, the blood in your urine should clear; if it does not, seek medical attention.
You may experience various emotions; some men feel ready to get going with life, while others think they need to take a break to recover fully. It is expected to feel less optimistic, tired, and easily fatigued on some days. Take power naps and remind yourself that this is a temporary, normal feeling/s.
How soon can I drive after TURP?
You will need to feel comfortable wearing a seatbelt and be able to do an emergency stop. This is the recommendation by the Driver and Vehicle Licensing Agency (DVLA).
Inform your insurance company to check when you are covered before going behind the wheel.