The National Cancer Institute recognises the role of hormone therapy in men with metastatic prostate cancer, locally advanced prostate cancer or localised prostate cancer.
Hormone therapy, also known as androgen deprivation therapy (ADT), is vital in managing and treating hormone-sensitive prostate cancer.
What is testosterone?
Testosterone is a hormone primarily produced in the testes of males. The testosterone production process involves a complex system that begins in the brain and affects several glands and organs. Here's a simplified explanation of how testosterone is produced in males:
- Hypothalamus: The process starts in the hypothalamus, a brain region that releases gonadotropin-releasing hormone (GnRH). GnRH acts as a signal to stimulate the pituitary gland.
- Pituitary gland: In response to GnRH, the pituitary gland, located at the base of the brain, releases two hormones called luteinizing hormone (LH) and follicle-stimulating hormone (FSH) into the bloodstream.
- Testes: LH travels through the bloodstream to the testes, stimulating specialised Leydig cells. Leydig cells are responsible for producing testosterone. LH binds to receptors on Leydig cells, triggering the production and release of testosterone.
- Testosterone production: In Leydig cells, reactions occur to convert cholesterol into testosterone. This process is known as steroidogenesis. Testosterone is then released into the bloodstream.
- Feedback loop: This maintains the balance of testosterone production in the body.
It is important to note that testosterone production is not limited to the testes. Small amounts of testosterone are also produced in the adrenal glands on top of the kidneys. However, the majority of testosterone is derived from the testes.
Testosterone plays a crucial role in various aspects of male health, including developing and maintaining sexual characteristics, muscle mass, bone density, and overall well-being.
Types of hormone therapy:
Hormone therapy for prostate cancer treatment involves targeting and reducing the levels of androgens, such as testosterone, in the body. There are various approaches to achieve this, including:
a) Orchidectomy (surgical castration): Orchidectomy involves the surgical removal of the testicles, the primary source of testosterone production in men. By eliminating the source of testosterone, orchidectomy effectively reduces androgen levels in the body. Nowadays, this is reserved for very elderly men or those men who are needle-phobic.
b) Treatment to lower androgen levels from other body parts: Aside from the testicles, other tissues in the body also contribute to androgen production. Medications can block the production of androgens in these tissues, such as the adrenal glands. This approach aims to inhibit the synthesis of androgens and lower their overall levels.
c) LHRH agonists and antagonists: Luteinizing hormone-releasing hormone (LHRH) agonists and antagonists are medicines that stop the testicles from making testosterone. LHRH agonists stimulate testosterone production before desensitising the receptors and reducing testosterone levels. On the other hand, LHRH antagonists directly block the receptors, leading to immediate testosterone suppression.
How is hormone therapy used to treat hormone-sensitive prostate cancer?
Hormone therapy is employed as a primary treatment for hormone-sensitive prostate cancer, aiming to suppress the growth and spread of cancer cells. It can be used in several ways:
a) Neoadjuvant therapy: Hormone therapy may be administered before other treatments, such as radiation therapy, to shrink the tumour and make subsequent interventions more effective.
b) Adjuvant therapy: After primary treatments like surgery or radiation therapy, hormone therapy may be utilised to reduce the risk of cancer recurrence by targeting any remaining cancer cells.
c) Palliative therapy: In advanced cases or when prostate cancer has metastasised, hormone therapy can help alleviate symptoms, slow the progression of the disease, and improve the patient's quality of life.
What can be done to reduce the side effects of hormone therapy for prostate cancer?
While hormone therapy is highly effective in managing hormone-sensitive prostate cancer, it can also be associated with various side effects. These may include:
a) Sexual dysfunction: Hormone therapy can reduce sexual desire (libido), erectile dysfunction, and loss of spontaneous erections. These effects may be temporary or persistent.
b) Hot flashes: Many men undergoing hormone therapy experience hot flashes, which are sudden sensations of heat and sweating. These can be managed through lifestyle modifications and medications.
c) Loss of bone density: Hormone therapy can weaken the bones and increase the risk of osteoporosis and fractures. Regular exercise, calcium, vitamin D supplementation, and periodic bone density monitoring can help mitigate this risk.
d) Fatigue and mood changes: Hormone therapy may cause fatigue, depression, or mood swings. Engaging in regular physical activity, maintaining a healthy diet, and seeking support from healthcare professionals or support groups can assist in coping with these challenges.
Heart disease: randomized clinical trials have shown a link between hormone therapy for prostate cancer cells and increased risk of heart disease. A healthy diet, regular exercise, and close monitoring of cholesterol and diabetes are key.
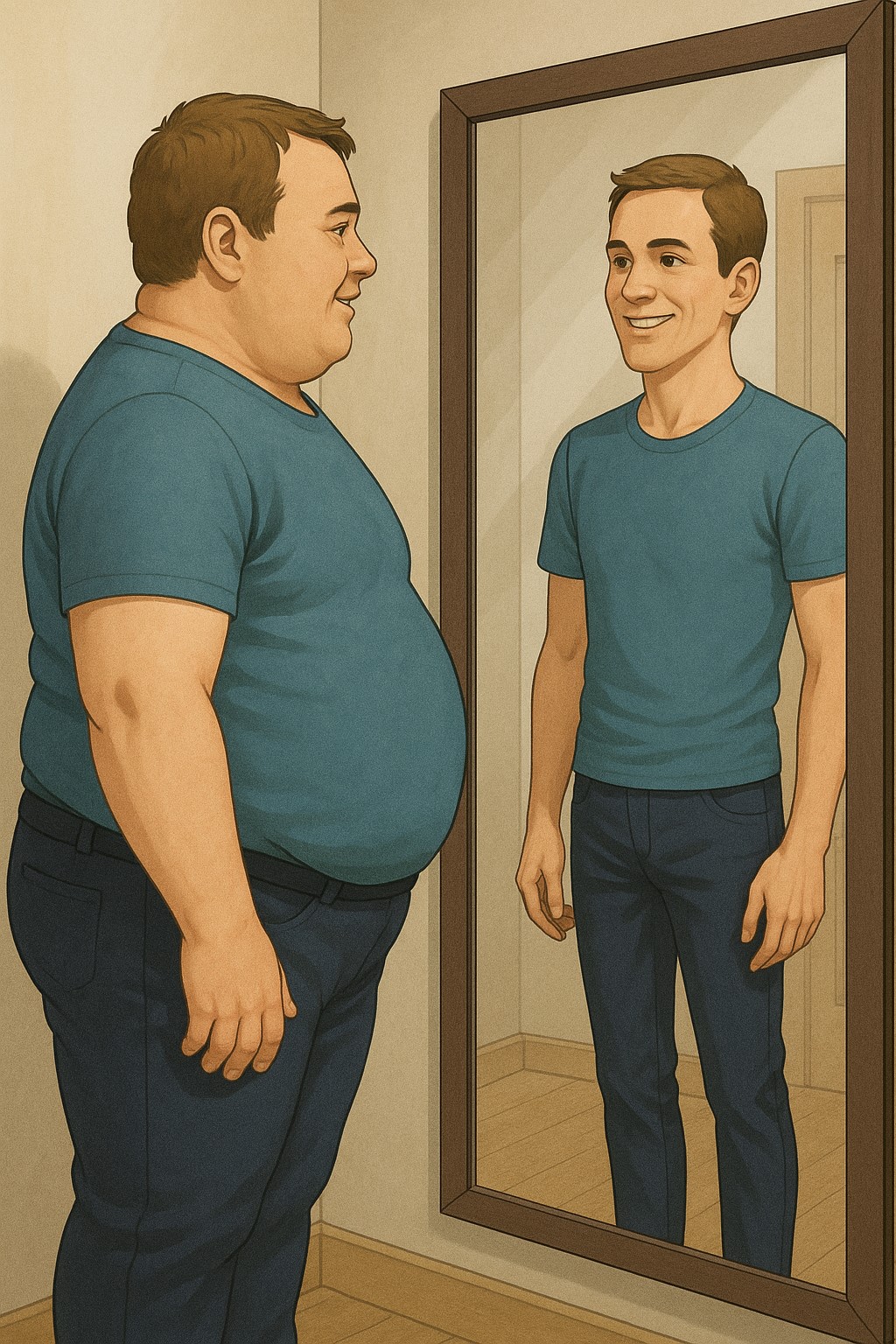
e) Weight gain: Hormone therapy can contribute to weight gain and changes in body composition. A balanced diet and regular exercise can help manage weight and minimise side effects.
Androgens and prostate physiology:
Androgens, particularly testosterone, play a crucial role in prostate physiology and the development of prostate cancer. The growth and proliferation of prostate cells depend on androgens binding to androgen receptors within the cells. By reducing androgen levels or blocking androgen receptors, hormone therapy inhibits prostate cancer cell growth and slows disease progression.
How will I know that my hormone therapy is working?
Monitoring the effectiveness of hormone therapy is essential to ensure optimal management of prostate cancer. Prostate specialists employ several methods to evaluate treatment response, including:
a) Prostate-specific antigen (PSA) levels: PSA is a protein produced by the prostate gland, and its levels can indicate the presence and progression of prostate cancer. Decreasing or stabilising PSA levels at lower levels generally shows a positive response to hormone therapy.
b) Imaging tests: Imaging techniques, such as bone or computed tomography (CT) scans and PSMA, may be utilised to assess the extent of disease spread or detect any metastases. A reduction in tumour size or absence of new lesions suggests a favourable treatment response.
c) Clinical evaluation: Improvement in symptoms, stabilisation of the disease, or prolonged survival are positive indicators of treatment efficacy.
Treating early-stage cancer:
For patients with early-stage prostate cancer, initiating hormone therapy requires careful consideration. Factors such as tumour aggressiveness, patient age, overall health status, and patient preferences should be considered. In some cases, active surveillance or watchful waiting may be appropriate, deferring hormone therapy until necessary. However, hormone therapy may be initiated alongside other treatments, such as radiation therapy or surgery, for high-risk or aggressive tumours to optimise outcomes.
Intermittent versus continuous hormone therapy:
Intermittent hormone therapy is an alternative approach to continuous androgen deprivation. It involves cycles of hormone therapy, with treatment periods followed by breaks. This approach aims to minimize side effects and improve quality of life while maintaining disease control. Research studies have shown that intermittent hormone therapy can be as effective as continuous therapy in selected patients while providing periods of respite from treatment-related side effects.
How is castration-resistant prostate cancer treated?
Despite the initial effectiveness of hormone therapy, some prostate cancers may eventually resist this treatment approach. This is known as castration-resistant prostate cancer (CRPC). Several treatment options are available for CRPC, including:
a) Chemotherapy: Docetaxel and cabazitaxel are chemotherapy drugs used to treat metastatic castration-resistant prostate cancer (mCRPC). They function by inhibiting cell division and growth, impeding cancer progression. Clinical trials have demonstrated their efficacy in extending overall survival and improving quality of life in mCRPC patients. Docetaxel is typically administered intravenously every three weeks, while cabazitaxel is administered every three weeks in combination with prednisone or prednisolone. Common side effects of both drugs include fatigue, hair loss, nausea, and low blood cell counts. Docetaxel is considered a first-line treatment, while cabazitaxel is typically used in patients who have already received docetaxel or progressed after docetaxel treatment
b) New treatments: Abiraterone acetate and enzalutamide are approved medicines that can be taken by mouth to treat mCRPC, which is prostate cancer that has spread and is no longer responding to hormone therapy. Abiraterone acetate inhibits the production of androgens (male hormones) in the body, including within the tumour cells. Enzalutamide works by blocking the androgen receptors, preventing the binding and activation of androgens. Clinical trials have shown that both drugs extend overall survival, delay disease progression, and improve quality of life in mCRPC patients. Abiraterone acetate is typically taken with prednisone to minimize side effects, while enzalutamide is a standalone therapy. Common side effects of abiraterone acetate include fluid retention, high blood pressure, and liver enzyme elevation. Enzalutamide's side effects may include fatigue, hot flashes, and cognitive changes. These medications are often used in the later stages of prostate cancer, either as initial treatment for mCRPC or following the progression of the disease after other therapies. To ensure the best course of action for each patient, healthcare professionals with expertise in oncology should tailor treatment plans.
c) Sipuleucel-T (Provenge) is an immunotherapy for metastatic castration-resistant prostate cancer (mCRPC). It stimulates the patient's immune system to target cancer cells. The treatment involves leukapheresis. Sipuleucel-T activates an immune response, activating T cells and destroying prostate cancer cells. Clinical trials have shown improved overall survival in mCRPC patients. Common side effects include chills, fatigue, fever, and nausea. Sipuleucel-T is approved explicitly for asymptomatic or minimally symptomatic mCRPC.
If you have metastatic castration-resistant prostate cancer (mCRPC) that has spread to your bones, Radium-223 (Xofigo) is a targeted alpha therapy that can help. It delivers radiation directly to bone metastases, selectively targeting cancer cells while minimizing damage to surrounding healthy tissues. Clinical trials have demonstrated its ability to extend overall survival and improve quality of life in patients with mCRPC and bone metastases. Administered through intravenous injections once every four weeks for six injections, Radium-223 has shown efficacy in relieving pain and delaying skeletal-related events. Common side effects include nausea, diarrhoea, vomiting, and low blood cell counts. It is specifically indicated for mCRPC patients with symptomatic bone metastases and no known visceral metastases. Radium-223 can be used alone or with other treatments, such as hormone therapy, and precautions are taken to minimize radiation exposure. Consulting healthcare professionals is essential for personalized treatment plans and a comprehensive understanding of Radium-223.
Combined androgen blockade (CAB):
This approach aims to achieve a more comprehensive and potent suppression of androgen activity. A common method used in CAB is to mix an LHRH agonist or antagonist with an anti-androgen drug, like bicalutamide or flutamide. Compared to monotherapy alone, studies have shown that CAB can improve PSA response rates and overall survival.
Low testosterone and prostate cancer risk:
Lower testosterone levels have been associated with a reduced risk of developing prostate cancer. This observation has led to investigations into using testosterone-lowering therapies, such as androgen deprivation, to prevent prostate cancer.
However, the role of testosterone-lowering therapy in prostate- cancer treatment and prevention is still being studied, and further research is needed to establish its efficacy and long-term effects.
Endogenous testosterone in prostate cancer patients:
While hormone therapy aims to reduce testosterone levels, it's important to note that complete androgen deprivation is often not achieved. Small amounts of testosterone can still be produced within the body, even during hormone therapy. This residual testosterone, though significantly reduced, may contribute to the development of castration-resistant prostate cancer. Researchers are working hard to figure out how to stop the production of testosterone and come up with ways to target this residual androgen activity.
Prostate cancer and testosterone levels in men who are on testosterone replacement therapy
Some studies have suggested that the risk of prostate cancer may increase right after starting testosterone therapy and then plateau or decline over time. However, other studies have found no significant association between testosterone therapy and prostate cancer risk.
The relationship between testosterone therapy and the risk of prostate cancer is still not fully understood. While some studies suggest a potential association, there is no conclusive evidence to establish a direct cause-and-effect relationship. Close monitoring (blood testosterone levels) and regular follow-up with a healthcare professional is vital.
Reflection from a prostate cancer urologist
Hormone therapy, or androgen deprivation therapy, is pivotal in treating hormone-sensitive prostate cancer. Various approaches, including surgical and medical interventions, are utilized to reduce androgen levels and inhibit the growth of prostate cancer cells. Monitoring treatment response, managing side effects, and considering alternative therapies for castration-resistant disease are essential aspects of prostate cancer management. As research advances, new treatment strategies are being developed to improve outcomes and enhance the quality of life for individuals affected by prostate cancer.